Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
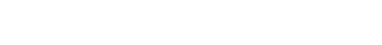
- Efficacy and Safety of Omarigliptin, a Novel Once-Weekly Dipeptidyl Peptidase-4 Inhibitor, in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis
- A.B.M. Kamrul-Hasan, Muhammad Shah Alam, Samir Kumar Talukder, Deep Dutta, Shahjada Selim
- Endocrinol Metab. 2024;39(1):109-126. Published online January 23, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1839
- 1,321 View
- 47 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
No recent meta-analysis has holistically analyzed and summarized the efficacy and safety of omarigliptin in type 2 diabetes mellitus (T2DM). We conducted a meta-analysis to address this knowledge gap.
Methods
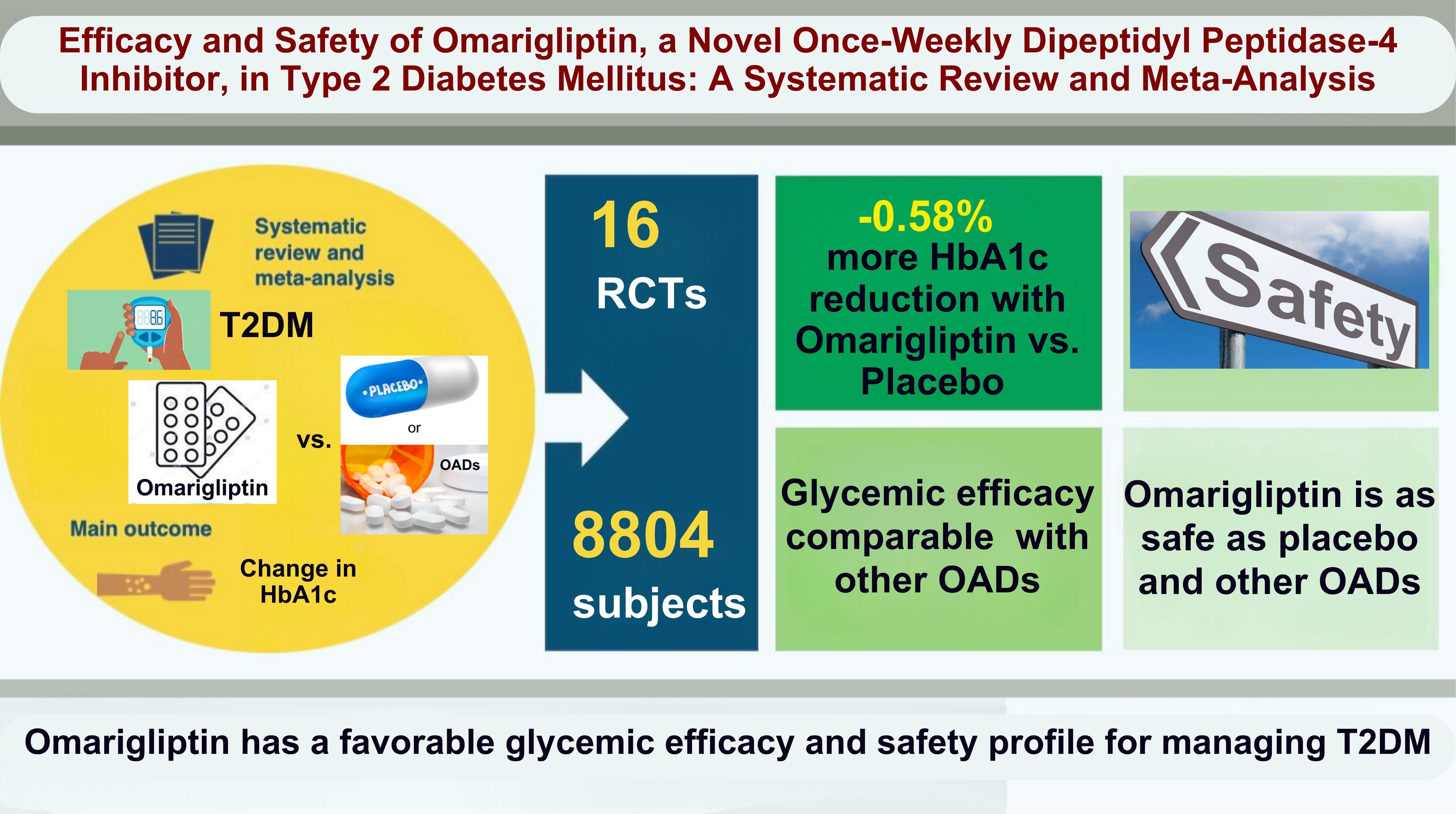
Electronic databases were searched to identify randomized controlled trials (RCTs) that included patients with T2DM who received omarigliptin in the intervention arm. The control arm consisted of either a placebo (passive control group [PCG]) or an active comparator (active control group [ACG]). The primary outcome assessed was changes in hemoglobin A1c (HbA1c), while secondary outcomes included variations in glucose levels, achievement of glycemic targets, adverse events (AEs), and hypoglycemic events.
Results
From 332 initially screened articles, data from 16 RCTs involving 8,804 subjects were analyzed. Omarigliptin demonstrated superiority over placebo in reducing HbA1c levels (mean difference, –0.58%; 95% confidence interval, –0.75 to –0.40; P<0.00001; I2=91%). Additionally, omarigliptin outperformed placebo in lowering fasting plasma glucose, 2-hour postprandial glucose, and in the percentage of participants achieving HbA1c levels below 7.0% and 6.5%. The glycemic efficacy of omarigliptin was similar to that of the ACG across all measures. Although the omarigliptin group experienced a higher incidence of hypoglycemic events compared to the PCG, the overall AEs, serious AEs, hypoglycemia, and severe hypoglycemia were comparable between the omarigliptin and control groups (PCG and ACG).
Conclusion
Omarigliptin has a favorable glycemic efficacy and safety profile for managing T2DM.

- Diabetes, obesity and metabolism
- Association between Serum Amyloid A Levels and Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis
- Ting Liu, Meng Li, Chunying Cui, Jielin Zhou
- Endocrinol Metab. 2023;38(3):315-327. Published online June 7, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1621

- 2,321 View
- 105 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
To date, consistent data have not been reported on the association between serum amyloid A (SAA) levels and type 2 diabetes mellitus (T2DM). The purpose of this study was to systematically summarize their relationship.
Methods
Databases including PubMed, Cochrane Library, Embase, Web of Science, and MEDLINE were searched until August 2021. Cross-sectional and case-control studies were included.
Results
Twenty-one studies with 1,780 cases and 2,070 controls were identified. SAA levels were significantly higher in T2DM patients than in healthy groups (standardized mean difference [SMD], 0.68; 95% confidence interval [CI], 0.39 to 0.98). A subgroup analysis showed that the mean age of participants and the continent that participants were from were related to differences in SAA levels between cases and controls. Furthermore, in T2DM patients, SAA levels were positively associated with body mass index (r=0.34; 95% CI, 0.03 to 0.66), triglycerides (r=0.12; 95% CI, 0.01 to 0.24), fasting plasma glucose (r=0.26; 95% CI, 0.07 to 0.45), hemoglobin A1c (r=0.24; 95% CI, 0.16 to 0.33), homeostasis model assessment for insulin resistance (r=0.22; 95% CI, 0.10 to 0.34), C-reactive protein (r=0.77; 95% CI, 0.62 to 0.91), and interleukin-6 (r=0.42; 95% CI, 0.31 to 0.54), but negatively linked with highdensity lipoprotein cholesterol (r=–0.23; 95% CI, –0.44 to –0.03).
Conclusion
The meta-analysis suggests that high SAA levels may be associated with the presence of T2DM, as well as lipid metabolism homeostasis and the inflammatory response. -
Citations
Citations to this article as recorded by- Correlation between insulin resistance and the rate of neutrophils-lymphocytes, monocytes-lymphocytes, platelets-lymphocytes in type 2 diabetic patients
Yuanyuan Zhang, Huaizhen Liu
BMC Endocrine Disorders.2024;[Epub] CrossRef - Antioxidant and Anti-Inflammatory Functions of High-Density Lipoprotein in Type 1 and Type 2 Diabetes
Damien Denimal
Antioxidants.2023; 13(1): 57. CrossRef
- Correlation between insulin resistance and the rate of neutrophils-lymphocytes, monocytes-lymphocytes, platelets-lymphocytes in type 2 diabetic patients

- Thyroid
Thyroid Cancer Screening - Diagnostic Performance of Ultrasound-Based Risk Stratification Systems for Thyroid Nodules: A Systematic Review and Meta-Analysis
- Leehi Joo, Min Kyoung Lee, Ji Ye Lee, Eun Ju Ha, Dong Gyu Na
- Endocrinol Metab. 2023;38(1):117-128. Published online February 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1670

- 2,343 View
- 170 Download
- 3 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study investigated the diagnostic performance of biopsy criteria in four society ultrasonography risk stratification systems (RSSs) for thyroid nodules, including the 2021 Korean (K)-Thyroid Imaging Reporting and Data System (TIRADS).
Methods
The Ovid-MEDLINE, Embase, Cochrane, and KoreaMed databases were searched and a manual search was conducted to identify original articles investigating the diagnostic performance of biopsy criteria for thyroid nodules (≥1 cm) in four widely used society RSSs.
Results
Eleven articles were included. The pooled sensitivity and specificity were 82% (95% confidence interval [CI], 74% to 87%) and 60% (95% CI, 52% to 67%) for the American College of Radiology (ACR)-TIRADS, 89% (95% CI, 85% to 93%) and 34% (95% CI, 26% to 42%) for the American Thyroid Association (ATA) system, 88% (95% CI, 81% to 92%) and 42% (95% CI, 22% to 67%) for the European (EU)-TIRADS, and 96% (95% CI, 94% to 97%) and 21% (95% CI, 17% to 25%) for the 2016 K-TIRADS. The sensitivity and specificity were 76% (95% CI, 74% to 79%) and 50% (95% CI, 49% to 52%) for the 2021 K-TIRADS1.5 (1.5-cm size cut-off for intermediate-suspicion nodules). The pooled unnecessary biopsy rates of the ACR-TIRADS, ATA system, EU-TIRADS, and 2016 K-TIRADS were 41% (95% CI, 32% to 49%), 65% (95% CI, 56% to 74%), 68% (95% CI, 60% to 75%), and 79% (95% CI, 74% to 83%), respectively. The unnecessary biopsy rate was 50% (95% CI, 47% to 53%) for the 2021 K-TIRADS1.5.
Conclusion
The unnecessary biopsy rate of the 2021 K-TIRADS1.5 was substantially lower than that of the 2016 K-TIRADS and comparable to that of the ACR-TIRADS. The 2021 K-TIRADS may help reduce potential harm due to unnecessary biopsies. -
Citations
Citations to this article as recorded by- Accuracy of ultrasound in predicting thyroid malignancy: a comparative analysis of the ACR TI-RADS and ATA risk stratification systems
Shaza Samargandy, Aliaa H. Ghoneim
Archives of Endocrinology and Metabolism.2024;[Epub] CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - The 2017 United States Preventive Services Task Force Recommendation for Thyroid Cancer Screening Is No Longer the Gold Standard
Ka Hee Yi
Endocrinology and Metabolism.2023; 38(1): 72. CrossRef - Thyroid Cancer Screening: How to Maximize Its Benefits and Minimize Its Harms
Jung Hwan Baek
Endocrinology and Metabolism.2023; 38(1): 75. CrossRef - 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules
Young Joo Park, Eun Kyung Lee, Young Shin Song, Soo Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung
International Journal of Thyroidology.2023; 16(1): 1. CrossRef - Evaluation of the Appropriateness of Thyroid Fine-Needle Aspiration
Lairce Cristina Ribeiro Brito, Iara Beatriz De Carvalho Botêlho, Lanna Matos Silva Fernandes, Nayze Lucena Sangreman Aldeman, Uziel Nunes Silva
International Journal for Innovation Education and Research.2023; 11(6): 8. CrossRef
- Accuracy of ultrasound in predicting thyroid malignancy: a comparative analysis of the ACR TI-RADS and ATA risk stratification systems

- Calcium & Bone Metabolism
- Effect of Vitamin D Supplementation on Risk of Fractures and Falls According to Dosage and Interval: A Meta-Analysis
- Sung Hye Kong, Han Na Jang, Jung Hee Kim, Sang Wan Kim, Chan Soo Shin
- Endocrinol Metab. 2022;37(2):344-358. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1374
- 6,342 View
- 282 Download
- 16 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Although recent studies comparing various dosages and intervals of vitamin D supplementation have been published, it is yet to be elucidated whether there is an appropriate dose or interval to provide benefit regarding fracture risk. We aimed to assess the published evidence available to date regarding the putative beneficial effects of vitamin D supplements on fractures and falls according to various dosages and intervals.
Methods
We performed a meta-analysis of randomized controlled studies reporting associations between vitamin D supplementation and the risks of fractures and falls in PubMed, EMBASE, and Cochrane library. Studies with supplements of ergocalciferol or calcitriol, those with a number of event ≤10, or those with a follow-up duration of less than 6 months were also excluded.
Results
Thirty-two studies were included in the final analysis. Vitamin D supplementation with daily dose of 800 to 1,000 mg was associated with lower risks of osteoporotic fracture and fall (pooled relative risk [RR], 0.87; 95% confidence interval [CI], 0.78 to 0.97 and RR, 0.91; 95% CI, 0.85 to 0.98), while studies with <800 or >1,000 mg/day did not. Also, among intervals, daily administration of vitamin D was associated with the reduced risk of falls, while intermittent dose was not. Also, patients with vitamin D deficiency showed a significant risk reduction of falls after vitamin D supplementation.
Conclusion
Daily vitamin D dose of 800 to 1,000 IU was the most probable way to reduce the fracture and fall risk. Further studies designed with various regimens and targeted vitamin D levels are required to elucidate the benefits of vitamin D supplements. -
Citations
Citations to this article as recorded by- Ukrainian Consensus on Diagnosis and Management of Vitamin D Deficiency in Adults
Nataliia Grygorieva, Mykola Tronko, Volodymir Kovalenko, Serhiy Komisarenko, Tetiana Tatarchuk, Ninel Dedukh, Mykola Veliky, Serhiy Strafun, Yulia Komisarenko, Andrii Kalashnikov, Valeria Orlenko, Volodymyr Pankiv, Oleg Shvets, Inna Gogunska, Svitlana Reg
Nutrients.2024; 16(2): 270. CrossRef - Vitamin D Supplementation: A Review of the Evidence Arguing for a Daily Dose of 2000 International Units (50 µg) of Vitamin D for Adults in the General Population
Pawel Pludowski, William B. Grant, Spyridon N. Karras, Armin Zittermann, Stefan Pilz
Nutrients.2024; 16(3): 391. CrossRef - Clinical Characteristics and Outcomes of Limb Fractures in Saudi Children
Lamia Aldhbiban, Fai Alhoshan, Raghad Alomari, Shahad A Almatrafi, Yousef Alanazi, Samir Alsayegh, Haifa Y Alfaraidi, Ayman H Jawadi, Fahad N Aljuraibah
Cureus.2024;[Epub] CrossRef - The interplay of rheumatoid arthritis and osteoporosis: exploring the pathogenesis and pharmacological approaches
Nikhil Gupta, Navjot Kanwar, Anchal Arora, Kavin Khatri, Abhinav Kanwal
Clinical Rheumatology.2024; 43(5): 1421. CrossRef - The multi-faceted nature of age-associated osteoporosis
A.E. Smit, O.C. Meijer, E.M. Winter
Bone Reports.2024; 20: 101750. CrossRef - Vitamin D Deficiency in Patients With Low-Energy Hip Fractures in Accordance With the Mediterranean Paradox
Christos Konstantinidis, Ourania Psoma, Christos Kotsias, Vasileios Panagiotopoulos , Sotiris Plakoutsis, Dimitrios Tsiampas, Dimitrios Vardakas, Dimitrios Giotis
Cureus.2024;[Epub] CrossRef - Effect of vitamin D, calcium, or combined supplementation on fall prevention: a systematic review and updated network meta-analysis
Long Tan, Ruiqian He, Xiaoxue Zheng
BMC Geriatrics.2024;[Epub] CrossRef - Association of vitamin and/or nutritional supplements with fall among patients with diabetes: A prospective study based on ACCORD and UK Biobank
Lingfang He, Tianqi Ma, Guogang Zhang, Xunjie Cheng, Yongping Bai
Frontiers in Nutrition.2023;[Epub] CrossRef - Vitamin D and Calcium in Osteoporosis, and the Role of Bone Turnover Markers: A Narrative Review of Recent Data from RCTs
Gavriela Voulgaridou, Sousana K. Papadopoulou, Paraskevi Detopoulou, Despoina Tsoumana, Constantinos Giaginis, Foivi S. Kondyli, Evgenia Lymperaki, Agathi Pritsa
Diseases.2023; 11(1): 29. CrossRef - Recent advances in the identification of related factors and preventive strategies of hip fracture
Yaohui Yu, Yudan Wang, Xiaoli Hou, Faming Tian
Frontiers in Public Health.2023;[Epub] CrossRef - Can Nutrition Contribute to a Reduction in Sarcopenia, Frailty, and Comorbidities in a Super-Aged Society?
Sadao Yoshida, Ryo Shiraishi, Yuki Nakayama, Yasuko Taira
Nutrients.2023; 15(13): 2991. CrossRef - Safety Profile of Vitamin D in Italy: An Analysis of Spontaneous Reports of Adverse Reactions Related to Drugs and Food Supplements
Valentina Maggini, Giada Crescioli, Ilaria Ippoliti, Eugenia Gallo, Francesca Menniti-Ippolito, Adelaide Chiaravalloti, Vittorio Mascherini, Roberto Da Cas, Simona Potenza, Giulia Gritti, Maria Galiulo, Laura Sottosanti, Alfredo Vannacci, Niccolò Lombardi
Journal of Clinical Medicine.2023; 12(14): 4726. CrossRef - Cholecalciferol Use Is Associated With a Decreased Risk of Incident Morphometric Vertebral Fractures in Acromegaly
Sabrina Chiloiro, Stefano Frara, Irene Gagliardi, Antonio Bianchi, Antonella Giampietro, Margherita Medici, Agnese Allora, Luigi di Filippo, Maria Rosaria Ambrosio, Alfredo Pontecorvi, Maria Chiara Zatelli, Laura De Marinis, Andrea Giustina
The Journal of Clinical Endocrinology & Metabolism.2023; 109(1): e58. CrossRef - Proceedings of the 2023 Santa Fe Bone Symposium: Progress and Controversies in the Management of Patients with Skeletal Diseases
E. Michael Lewiecki, Teresita Bellido, John P. Bilezikian, Jacques P. Brown, Azeez Farooki, Christopher S. Kovacs, Brendan Lee, William D. Leslie, Michael R. McClung, Mark L. Prasarn, Deborah E. Sellmeyer
Journal of Clinical Densitometry.2023; 26(4): 101432. CrossRef - Diagnosis, prevention and treatment of vitamin D deficiency in adults: Ukrainian experts consensus statement
N.V. Grygorieva, M.D. Tronko, V.M. Kovalenko, S.V. Komisarenko, T.F. Tatarchuk, N.V. Dedukh, M.M. Veliky, S.S. Strafun, Y.I. Komisarenko, A.V. Kalashnikov, V.L. Orlenko, V.I. Pankiv, O.V. Shvets, I.V. Gogunska, S.I. Regeda
PAIN, JOINTS, SPINE.2023; 13(2): 60. CrossRef - Serum 25-Hydroxyvitamin D Level Is Negatively Associated with Fatigue in Elderly Maintenance Hemodialysis Patients
Menglin Pang, Lin Chen, Na Jiang, Mengmeng Jiang, Baofeng Wang, Lili Wang, Xiao-yan Jia
Kidney and Blood Pressure Research.2023; 48(1): 231. CrossRef - Vitamin D for Clinical Diseases in Women: An Indispensable Factor in Medicine and Dentistry
Dario Calafiore, Leonzio Fortunato, Mario Migliario
Journal of Clinical Medicine.2022; 11(11): 3104. CrossRef - Malnutrition in Older Adults—Effect on Falls and Fractures: A Narrative Review
Malgorzata Kupisz-Urbanska, Ewa Marcinowska-Suchowierska
Nutrients.2022; 14(15): 3123. CrossRef - Role of vitamin D supplementation in the management of musculoskeletal diseases: update from an European Society of Clinical and Economical Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) working group
Thierry Chevalley, Maria Luisa Brandi, Kevin D. Cashman, Etienne Cavalier, Nicholas C. Harvey, Stefania Maggi, Cyrus Cooper, Nasser Al-Daghri, Oliver Bock, Olivier Bruyère, Mario Miguel Rosa, Bernard Cortet, Alfonso J. Cruz-Jentoft, Antonio Cherubini, Bes
Aging Clinical and Experimental Research.2022; 34(11): 2603. CrossRef - The Relationship of Osteoporosis with Menopause: Review of Article
Hadeel Anwar Alsarraje, *Liqaa Khalel Alhyali
International Journal of Research in Medical Sciences and Technology.2022; 14(01): 127. CrossRef
- Ukrainian Consensus on Diagnosis and Management of Vitamin D Deficiency in Adults

- Diabetes, Obesity and Metabolism
- Efficacy and Safety of the New Appetite Suppressant, Liraglutide: A Meta-Analysis of Randomized Controlled Trials
- Shinje Moon, Jibeom Lee, Hye Soo Chung, Yoon Jung Kim, Jae Myung Yu, Sung Hoon Yu, Chang-Myung Oh
- Endocrinol Metab. 2021;36(3):647-660. Published online June 18, 2021
- DOI: https://doi.org/10.3803/EnM.2020.934

- 6,286 View
- 302 Download
- 13 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity is a chronic disease associated with metabolic diseases such as diabetes and cardiovascular disease. Since the U.S. Food and Drug Administration approved liraglutide as an anti-obesity drug for nondiabetic patients in 2014, it has been widely used for weight control in overweight and obese people. This study aimed to systematically analyze the effects of liraglutide on body weight and other cardiometabolic parameters.
Methods
We investigated articles from PubMed, EMBASE, and the Cochrane Library to search randomized clinical trials that examined body weight changes with liraglutide treatment.
Results
We included 31 studies with 8,060 participants for this meta-analysis. The mean difference (MD) between the liraglutide group and the placebo group was −4.19 kg (95% confidence interval [CI], −4.84 to −3.55), with a −4.16% change from the baseline (95% CI, −4.90 to −3.43). Liraglutide treatment correlated with a significantly reduced body mass index (MD: −1.55; 95% CI, −1.76 to −1.34) and waist circumference (MD: −3.11 cm; 95% CI, −3.59 to −2.62) and significantly decreased blood pressure (systolic blood pressure, MD: −2.85 mm Hg; 95% CI, −3.36 to −2.35; diastolic blood pressure, MD: −0.66 mm Hg; 95% CI, −1.02 to −0.30), glycated hemoglobin (MD: −0.40%; 95% CI, −0.49 to −0.31), and low-density lipoprotein cholesterol (MD: –2.91 mg/dL; 95% CI, −5.28 to −0.53; MD: −0.87% change from baseline; 95% CI, −1.17 to −0.56).
Conclusion
Liraglutide is effective for weight control and can be a promising drug for cardiovascular protection in overweight and obese people. -
Citations
Citations to this article as recorded by- Pharmacotherapy for obesity: moving towards efficacy improvement
Walmir Coutinho, Bruno Halpern
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Physiopathology and Treatment of Obesity and Overweight: A Proposal for a New Anorectic
Bruno Silvestrini, Mauro Silvestrini, Mayank Choubey
Journal of Obesity.2024; 2024: 1. CrossRef - Side effect profile of pharmacologic therapies for liver fibrosis in nonalcoholic fatty liver disease: a systematic review and network meta-analysis
Yilin Li, Rong Lei, Honglin Lei, Qin Xiong, Fengjiao Xie, Chengjiao Yao, Peimin Feng
European Journal of Gastroenterology & Hepatology.2023; 35(1): 1. CrossRef - Recommendations for the prevention and management of obesity in the Iraqi population
Hussein Ali Nwayyir, Esraa Majid Mutasher, Osama Mohammed Alabid, Muthana Abdulrazzaq Jabbar, Wefak Hasan Abdulraheem Al-Kawaz, Haider Ayad Alidrisi, Majid Alabbood, Muhammed Chabek, Munib AlZubaidi, Lujain Anwar Al-khazrajy, Ibtihal Shukri Abd Alhaleem,
Postgraduate Medicine.2023; 135(5): 425. CrossRef - A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
Fatma Haddad, Ghadeer Dokmak, Maryam Bader, Rafik Karaman
Life.2023; 13(4): 1012. CrossRef - Liraglutide, a glucagon-like peptide-1 analog, in individuals with obesity in clinical practice
Juyoung Shin, Raeun Kim, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 49. CrossRef - The effects of subcutaneous Tirzepatide on obesity and overweight: a systematic review and meta‐regression analysis of randomized controlled trials
Pejman Rohani, Nasser Malekpour Alamdari, Seyedeh Elaheh Bagheri, Azita Hekmatdoost, Mohammad Hassan Sohouli
Frontiers in Endocrinology.2023;[Epub] CrossRef - Efficacy and safety of liraglutide for weight management in children and adolescents: a systematic review and meta-analysis of randomized controlled trials
Hao Gou, Yiman Zhai, Junjun Guo
European Journal of Pediatrics.2023; 182(11): 5095. CrossRef - Efficacy and safety of once-weekly semaglutide in adults with overweight or obesity: a meta-analysis
Ping Zhong, Hai Zeng, Miaochun Huang, Wenbin Fu, Zhixia Chen
Endocrine.2022; 75(3): 718. CrossRef - Pharmacological profile of once-weekly injectable semaglutide for chronic weight management
David C. W. Lau, Rachel L Batterham, Carel W. le Roux
Expert Review of Clinical Pharmacology.2022; 15(3): 251. CrossRef - Pharmacological Management of Obesity: A Century of Expert Opinions in Cecil Textbook of Medicine
Peter Manu, Cristina-Mihaela Lăcătuşu, Liliana M. Rogozea, Simona Cernea
American Journal of Therapeutics.2022; 29(4): e410. CrossRef - GLP-1 agonists: superior for mind and body in antipsychotic-treated patients?
Katerina Horska, Jana Ruda-Kucerova, Silje Skrede
Trends in Endocrinology & Metabolism.2022; 33(9): 628. CrossRef - Targeting skeletal muscle mitochondrial health in obesity
Chantal A. Pileggi, Breana G. Hooks, Ruth McPherson, Robert R.M. Dent, Mary-Ellen Harper
Clinical Science.2022; 136(14): 1081. CrossRef - A Study on Weight Loss Cause as per the Side Effect of Liraglutide
Jin Yu, Jeongmin Lee, Seung-Hwan Lee, Jae-Hyung Cho, Hun-Sung Kim, Heng Zhou
Cardiovascular Therapeutics.2022; 2022: 1. CrossRef
- Pharmacotherapy for obesity: moving towards efficacy improvement

- Clinical Study
- Efficacy and Safety of the Novel Dipeptidyl Peptidase-4 Inhibitor Gemigliptin in the Management of Type 2 Diabetes: A Meta-Analysis
- Deep Dutta, Anshita Agarwal, Indira Maisnam, Rajiv Singla, Deepak Khandelwal, Meha Sharma
- Endocrinol Metab. 2021;36(2):374-387. Published online April 6, 2021
- DOI: https://doi.org/10.3803/EnM.2020.818

- 6,563 View
- 226 Download
- 17 Web of Science
- 26 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
No meta-analysis has holistically analysed and summarised the efficacy and safety of gemigliptin in type 2 diabetes. The meta-analysis addresses this knowledge gap.
Methods
Electronic databases were searched for randomised controlled trials (RCTs) involving diabetes patients receiving gemigliptin in the intervention arm and placebo/active comparator in the control arm. The primary outcome was change in haemoglobin A1c (HbA1c). The secondary outcomes were alterations in glucose, glycaemic targets, lipids, insulin resistance, and adverse events.
Results
Data from 10 RCTs involving 1,792 patients were analysed. Four had an active control group (ACG), with metformin/dapagliflozin/sitagliptin/glimepiride as the active comparator; six had a passive control group (PCG), with placebo/rosuvastatin as controls. HbA1c reduction by gemigliptin at 24 weeks was comparable to ACG (mean difference [MD], 0.09%; 95% confidence interval [CI], –0.06 to 0.23; P=0.24; I2=0%; moderate certainty of evidence [MCE]), but superior to PCG (MD, –0.91%; 95% CI, –1.18 to –0.63); P<0.01; I2=89%; high certainty of evidence [HCE]). Gemigliptin was superior to PCG regarding achieving HbA1c <7% (12 weeks: odds ratio [OR], 5.91; 95% CI, 1.34 to 26.08; P=0.02; I2=74%; 24 weeks: OR, 4.48; 95% CI, 2.09 to 9.60; P<0.01; I2=69%; HCE). Gemigliptin was comparable to ACG regarding achieving HbA1c <7% after 24 weeks (OR, 0.92; 95% CI, 0.52 to 1.63; P=0.77; I2=66%; MCE). Adverse events were similar between the gemigliptin and control groups (risk ratio [RR], 1.06; 95% CI, 0.82 to 1.36; P=0.66; I2=35%; HCE). The gemigliptin group did not have increased hypoglycaemia (RR, 1.19; 95% CI, 0.62 to 2.28; P=0.61; I2=19%; HCE).
Conclusion
Gemigliptin has good glycaemic efficacy and is well-tolerated over 6 months of use. -
Citations
Citations to this article as recorded by- Hyperprolactinemia Due to Prolactinoma has an Adverse Impact on Bone Health with Predominant Impact on Trabecular Bone: A Systematic Review and Meta-Analysis
Lakshmi Nagendra, Deep Dutta, Sunetra Mondal, Nitin Kapoor, Ameya Joshi, Saptarshi Bhattacharya
Journal of Clinical Densitometry.2024; 27(1): 101453. CrossRef - Impact of early initiation of ezetimibe in patients with acute coronary syndrome: A systematic review and meta-analysis
Kunal Mahajan, Lakshmi Nagendra, Anil Dhall, Deep Dutta
European Journal of Internal Medicine.2024;[Epub] CrossRef - Efficacy and safety of dorzagliatin, a novel glucokinase activators, in the treatment of T2DM: A meta-analysis of randomized controlled trials
Yuqian Wu, Kai Wang, Jingyang Su, Xin Liu
Medicine.2024; 103(8): e36916. CrossRef - Glucagon-Like Peptide-1 Receptor Agonists in Post-bariatric Surgery Patients: A Systematic Review and Meta-analysis
Deep Dutta, Lakshmi Nagendra, Ameya Joshi, Suryashri Krishnasamy, Meha Sharma, Naresh Parajuli
Obesity Surgery.2024; 34(5): 1653. CrossRef - Orforglipron, a novel non‐peptide oral daily glucagon‐like peptide‐1 receptor agonist as an anti‐obesity medicine: A systematic review and meta‐analysis
Deep Dutta, Lakshmi Nagendra, Beatrice Anne, Manoj Kumar, Meha Sharma, A. B. M. Kamrul‐Hasan
Obesity Science & Practice.2024;[Epub] CrossRef - Safety and tolerability of sodium-glucose cotransporter-2 inhibitors in children and young adults: a systematic review and meta-analysis
Lakshmi Nagendra, Deep Dutta, Harish Bukkasagar Girijashankar, Deepak Khandelwal, Tejal Lathia, Meha Sharma
Annals of Pediatric Endocrinology & Metabolism.2024; 29(2): 82. CrossRef - Efficacy and safety of novel dual glucokinase activator dorzagliatin in type-2 diabetes A meta-analysis
Deep Dutta, Deepak Khandelwal, Manoj Kumar, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102695. CrossRef - Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Effects of Initial Combinations of Gemigliptin Plus Metformin Compared with Glimepiride Plus Metformin on Gut Microbiota and Glucose Regulation in Obese Patients with Type 2 Diabetes: The INTESTINE Study
Soo Lim, Minji Sohn, Jose C. Florez, Michael A. Nauck, Jiyoung Ahn
Nutrients.2023; 15(1): 248. CrossRef - Systematic review and meta-analysis of teneligliptin for treatment of type 2 diabetes
R. Pelluri, S. Kongara, V. R. Nagasubramanian, S. Mahadevan, J. Chimakurthy
Journal of Endocrinological Investigation.2023; 46(5): 855. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Verapamil improves One-Year C-Peptide Levels in Recent Onset Type-1 Diabetes: A Meta-Analysis
Deep Dutta, Lakshmi Nagendra, Nishant Raizada, Saptarshi Bhattacharya, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(3): 192. CrossRef - Role of novel sodium glucose co-transporter-2 inhibitor enavogliflozin in type-2 diabetes: A systematic review and meta-analysis
Deep Dutta, B.G. Harish, Beatrice Anne, Lakshmi Nagendra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(8): 102816. CrossRef - Semaglutide and cancer: A systematic review and meta-analysis
Lakshmi Nagendra, Harish BG, Meha Sharma, Deep Dutta
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(9): 102834. CrossRef - Efficacy and Safety of Novel Thiazolidinedione Rivoglitazone in Type-2 Diabetes a Meta-Analysis
Deep Dutta, Jyoti Kadian, Indira Maisnam, Ashok Kumar, Saptarshi Bhattacharya, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(4): 286. CrossRef - Impact of early initiation of proprotein convertase subtilisin/kexin type 9 inhibitors in patients with acute coronary syndrome: A systematic review meta-analysis
Lakshmi Nagendra, Kunal Mahajan, Gunjan Gupta, Deep Dutta
Indian Heart Journal.2023; 75(6): 416. CrossRef - Optimal use of once weekly icodec insulin in type-2 diabetes: An updated meta-analysis of phase-2 and phase-3 randomized controlled trials
Deep Dutta, Lakshmi Nagendra, Sowrabha Bhat, Ritin Mohindra, Vineet Surana, Anoop Misra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(10): 102877. CrossRef - Impact of Enhanced External Counter-pulsation Therapy on Glycaemic Control in People With Prediabetes and Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis
Lakshmi Nagendra, Deep Dutta, Meha Sharma, Harish Bg
touchREVIEWS in Endocrinology.2023; 19(2): 8. CrossRef - Role of Novel Glucagon-like Peptide-1 Receptor Analogue Polyethylene Glycol Loxenatide in Type 2 Diabetes: A Systematic Review and Meta-analysis
Deep Dutta, Subhankar Chatterjee, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(5): 377. CrossRef - Efficacy and Safety of Ultra-rapid Lispro Insulin in Managing Type-1 and Type-2 Diabetes: A Systematic Review and Meta-Analysis
Deep Dutta, Lakshmi Nagendra, Saptarshi Bhattacharya, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(6): 467. CrossRef - Safety and efficacy of once weekly dipeptidyl-peptidase-4 inhibitor trelagliptin in type-2 diabetes: A meta-analysis
Deep Dutta, Ritin Mohindra, Vineet Surana, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(4): 102469. CrossRef - Efficacy and safety of hydroxychloroquine for managing glycemia in type-2 diabetes: A systematic review and meta-analysis
D Dutta, R Jindal, D Mehta, M Kumar, M Sharma
Journal of Postgraduate Medicine.2022; 68(2): 85. CrossRef - Gemigliptin exerts protective effects against doxorubicin-induced hepatotoxicity by inhibiting apoptosis via the regulation of fibroblast growth factor 21 expression
Kyeong-Min Lee, Yeo Jin Hwang, Gwon-Soo Jung
Biochemical and Biophysical Research Communications.2022; 626: 135. CrossRef - Reporting and methodological quality of systematic reviews of DPP-4 inhibitors for patients with type 2 diabetes mellitus: an evidence-based mapping
Zouxi Du, Tingting Lu, Mingdong Gao, Limin Tian
Acta Diabetologica.2022; 59(12): 1539. CrossRef - Ranirestat improves electrophysiologic but not clinical measures of diabetic polyneuropathy: A meta-analysis
Deep Dutta, Ritin Mohindra, Manoj Kumar, Ashok Kumar, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2022; 26(5): 399. CrossRef - Efficacy and safety of novel twincretin tirzepatide a dual GIP and GLP-1 receptor agonist in the management of type-2 diabetes: A Cochrane meta-analysis
Deep Dutta, Vineet Surana, Rajiv Singla, Sameer Aggarwal, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2021; 25(6): 475. CrossRef
- Hyperprolactinemia Due to Prolactinoma has an Adverse Impact on Bone Health with Predominant Impact on Trabecular Bone: A Systematic Review and Meta-Analysis

- Clinical Study
- Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
- Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
- Endocrinol Metab. 2021;36(2):388-400. Published online March 31, 2021
- DOI: https://doi.org/10.3803/EnM.2020.912

- 6,426 View
- 361 Download
- 13 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To compare the renal effects of dipeptidyl peptidase-4 (DPP-4) inhibitors and sodium-glucose cotransporter 2 (SGLT2) inhibitors on individual outcomes in patients with type 2 diabetes.
Methods
We searched electronic databases (MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials) from inception to June 2019 to identity eligible randomized controlled trials of DPP-4 inhibitors or SGLT2 inhibitors that reported at least one kidney outcome in patients with type 2 diabetes. Outcomes of interest were microalbuminuria, macroalbuminuria, worsening nephropathy, and end-stage kidney disease (ESKD). We performed an arm-based network meta-analysis using Bayesian methods and calculated absolute risks and rank probabilities of each treatment for the outcomes.
Results
Seventeen studies with 87,263 patients were included. SGLT2 inhibitors significantly lowered the risks of individual kidney outcomes, including microalbuminuria (odds ratio [OR], 0.64; 95% credible interval [CrI], 0.41 to 0.93), macroalbuminuria (OR, 0.48; 95% CrI, 0.24 to 0.72), worsening nephropathy (OR, 0.65; 95% CrI, 0.44 to 0.91), and ESKD (OR, 0.65; 95% CrI, 0.46 to 0.98) as compared with placebo. However, DPP-4 inhibitors did not lower the risks. SGLT2 inhibitors were considerably associated with higher absolute risk reductions in all kidney outcomes than DPP-4 inhibitors, although the benefits were statistically insignificant. The rank probabilities showed that SGLT2 inhibitors were better treatments for lowering the risk of albuminuria and ESKD than placebo or DPP-4 inhibitors.
Conclusion
SGLT2 inhibitors were superior to DPP-4 inhibitors in reducing the risk of albuminuria and ESKD in patients with type 2 diabetes. -
Citations
Citations to this article as recorded by- Therapie des Typ-2-Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Die Diabetologie.2024; 20(2): 212. CrossRef - Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study
Mototsugu Nagao, Jun Sasaki, Kyoko Tanimura-Inagaki, Ichiro Sakuma, Hitoshi Sugihara, Shinichi Oikawa
Cardiovascular Diabetology.2024;[Epub] CrossRef - Comparative Effect of Glucose-Lowering Drugs for Type 2 Diabetes Mellitus on Stroke Prevention: A Systematic Review and Network Meta-Analysis
Ji Soo Kim, Gyeongsil Lee, Kyung-Il Park, Seung-Won Oh
Diabetes & Metabolism Journal.2024; 48(2): 312. CrossRef - Therapy of Type 2 Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Experimental and Clinical Endocrinology & Diabetes.2024;[Epub] CrossRef - Therapie des Typ-2-Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Die Diabetologie.2023; 19(5): 658. CrossRef - Renoprotective Effect of Thai Patients with Type 2 Diabetes Mellitus Treated with SGLT-2 Inhibitors versus DPP-4 Inhibitors: A Real-World Observational Study
Apichaya Chanawong, Suriyon Uitrakul, Supatcha Incomenoy, Natnicha Poonchuay, Rizky Abdulah
Advances in Pharmacological and Pharmaceutical Sciences.2023; 2023: 1. CrossRef - Different nursing interventions on sleep quality among critically ill patients: A systematic review and network meta-analysis
Daijin Huang, Yumei Li, Jing Ye, Chang Liu, Dongyan Shen, Yunhui Lv
Medicine.2023; 102(52): e36298. CrossRef - New trends in the approach to the treatment of type 2 diabetes - observations and benefits in the outpatient practice of a diabetologist
Pavel Weber, Hana Meluzínová, Dana Weberová
Klinická farmakologie a farmacie.2022; 35(4): 118. CrossRef - Comparative efficacy of novel antidiabetic drugs on cardiovascular and renal outcomes in patients with diabetic kidney disease: A systematic review and network meta‐analysis
Hongwei Cao, Tao Liu, Li Wang, Qiuhe Ji
Diabetes, Obesity and Metabolism.2022; 24(8): 1448. CrossRef - Therapie des Typ-2-Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Die Diabetologie.2022; 18(5): 623. CrossRef - Significant reduction in chronic kidney disease progression with sodium‐glucose cotransporter‐2 inhibitors compared to dipeptidyl peptidase‐4 inhibitors in adults with type 2 diabetes in a UK clinical setting: An observational outcomes study based on inte
Iskandar Idris, Ruiqi Zhang, Jil B. Mamza, Mike Ford, Tamsin Morris, Amitava Banerjee, Kamlesh Khunti
Diabetes, Obesity and Metabolism.2022; 24(11): 2138. CrossRef - Therapy of Type 2 Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Experimental and Clinical Endocrinology & Diabetes.2022; 130(S 01): S80. CrossRef - Molecular Mechanistic Pathways Targeted by Natural Compounds in the Prevention and Treatment of Diabetic Kidney Disease
Kaixuan Zhou, Xue Zi, Jiayu Song, Qiulu Zhao, Jia Liu, Huiwei Bao, Lijing Li
Molecules.2022; 27(19): 6221. CrossRef - Lower risk of gout in sodium glucose cotransporter 2 (SGLT2) inhibitors versus dipeptidyl peptidase-4 (DPP4) inhibitors in type-2 diabetes
Jiandong Zhou, Xuejin Liu, Oscar Hou-In Chou, Lifang Li, Sharen Lee, Wing Tak Wong, Qingpeng Zhang, Carlin Chang, Tong Liu, Gary Tse, Fengshi Jing, Bernard Man Yung Cheung
Rheumatology.2022;[Epub] CrossRef - New Era for Renal-Protective Therapy in Type 2 Diabetes: Better Renal Outcomes in Patients with Type 2 Diabetes Taking Sodium-Glucose Cotransporter 2 Inhibitors versus Dipeptidyl Peptidase-4 Inhibitors
Chan-Hee Jung
Endocrinology and Metabolism.2021; 36(2): 339. CrossRef - Efficacy / safety balance of DPP-4 inhibitors versus SGLT2 inhibitors in elderly patients with type 2 diabetes
André J. Scheen
Diabetes & Metabolism.2021; 47(6): 101275. CrossRef
- Therapie des Typ-2-Diabetes

- Clinical Study
- Efficacy of Ethanol Ablation for Benign Thyroid Cysts and Predominantly Cystic Nodules: A Systematic Review and Meta-Analysis
- Cheng-Chun Yang, Yung Hsu, Jyun-Yan Liou
- Endocrinol Metab. 2021;36(1):81-95. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2020.833

- 5,990 View
- 221 Download
- 11 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Ultrasound-guided minimally invasive procedures are widely used to treat thyroid diseases. The objective of this study was to assess the efficacy and safety of ethanol ablation (EA) in comparison with other non-surgical options in the treatment of benign thyroid cystic nodules.
Methods
We conducted a systematic search of studies on EA for thyroid cystic nodules, mainly in the Ovid-MEDLINE and Embase, Web of Science, and Cochrane databases. The standardized mean difference (SMD) of the volume reduction ratio (VRR) after EA versus other non-surgical treatments comprised the primary outcome, whereas the odds ratio (OR) of therapeutic success rates between the two groups comprised the secondary outcome.
Results
The meta-analysis included 19 studies (four randomized controlled trials and 15 non-randomized studies) with 1,514 participants. The cumulative VRR of EA was 83.908% (95% confidence interval [CI], 79.358% to 88.457%). EA had a significantly higher pooled VRR (SMD, 0.381; 95% CI, 0.028 to 0.734; P=0.030), but not a significantly higher pooled therapeutic success rate (OR, 0.867; 95% CI, 0.132 to 5.689; P=0.880), than other forms of non-surgical management including radiofrequency ablation (RFA), polidocanol sclerotherapy, and simple aspiration with or without saline flush. However, the VRR and therapeutic success rate were not significantly different between EA and RFA. Major complications were recorded only in six patients (0.53%) with self-limiting dysphonia.
Conclusion
The role of EA as the first-line treatment for benign thyroid cysts and predominantly cystic nodules is supported by its high effectiveness and good safety profile compared to other currently available non-surgical options. -
Citations
Citations to this article as recorded by- Ultrasound-guided ethanol ablation versus the Sistrunk operation as a primary treatment for thyroglossal duct cysts
Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee, Jin Ho Sohn
Ultrasonography.2024; 43(1): 25. CrossRef - The Comparison of Efficacy and Safety between Radiofrequency Ablation Alone and Ethanol Ablation Followed by Radiofrequency Ablation in the Treatment of Mixed Cystic and Solid Thyroid Nodule
Min Gang Jo, Min Kyoung Lee, Jae Ho Shin, Min Guk Seo, So Lyung Jung
Journal of the Korean Society of Radiology.2024;[Epub] CrossRef - Ultrasound-Guided Ethanol Ablation for Thyroglossal Duct Cyst: A Review of Technical Issues and Potential as a New Standard Treatment
Dongbin Ahn
Journal of Clinical Medicine.2023; 12(17): 5445. CrossRef - Ultrasound‐Guided Ethanol Ablation as a Primary Treatment for Thyroglossal Duct Cyst: Feasibility, Characteristics, and Outcomes
Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee, Jin Ho Sohn
Otolaryngology–Head and Neck Surgery.2023; 168(6): 1381. CrossRef - Ultraschallgeführte lokalablative Verfahren zur Behandlung von Schilddrüsenläsionen
Johannes-Paul Richter, Carl-Philip Richter, Daniel Gröner
Angewandte Nuklearmedizin.2023; 46(02): 169. CrossRef - A Case of Thyroid Abscess Following Ethanol Ablation for Benign Thyroid Nodule
Heungrae Cho, Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2023; 66(9): 624. CrossRef - Sclerotherapy with a Viscum Album Extract for the Two Patients with Cystic Thyroid Nodule
Jae Ha Lee, Seung Won Lee, Ki Nam Park
International Journal of Thyroidology.2023; 16(1): 139. CrossRef - Percutaneous ethanol injection in thyroid nodular pathology and metastatic cervical adenopathies: A systematic review, meta-analysis and economic evaluation
Beatriz León-Salas, Aránzazu Hernández-Yumar, Diego Infante-Ventura, Aythami de Armas Castellano, Yadira González Hernández, Renata Linertová, Teresa Téllez Santana, Pedro de Pablos-Velasco, María M. Trujillo-Martín
Endocrinología, Diabetes y Nutrición.2023; 70(9): 572. CrossRef - Ultraschallgeführte lokalablative Verfahren zur Behandlung von Schilddrüsenläsionen
Johannes-Paul Richter, Carl-Philip Richter, Daniel Gröner
Laryngo-Rhino-Otologie.2023; 102(12): 916. CrossRef - Percutaneous ethanol injection in thyroid nodular pathology and metastatic cervical adenopathies: A systematic review, meta-analysis and economic evaluation
Beatriz León-Salas, Aránzazu Hernández-Yumar, Diego Infante-Ventura, Aythami de Armas Castellano, Yadira González Hernández, Renata Linertová, Teresa Téllez Santana, Pedro de Pablos-Velasco, María M. Trujillo-Martín
Endocrinología, Diabetes y Nutrición (English ed.).2023; 70(9): 572. CrossRef - Safety and Efficacy of Ultrasound-Guided Radiofrequency Ablation for Benign Nonfunctional Thyroid Nodules in Children: A Retrospective Study of 62 Patients with Over Four Years of Follow-Up
Liwen Li, Xinguang Qiu
Thyroid.2022; 32(5): 525. CrossRef - Ethanol ablation for the treatment of benign thyroid nodules
Gabrielle K. Steinl, Latoya A. Stewart, Catherine McManus, James A. Lee, Jennifer H. Kuo
The American Journal of Surgery.2022; 224(1): 408. CrossRef - Minimally-invasive treatments for benign thyroid nodules: recommendations for information to patients and referring physicians by the Italian Minimally-Invasive Treatments of the Thyroid group
Giovanni Mauri, Stella Bernardi, Andrea Palermo, Roberto Cesareo, Enrico Papini, Luigi Solbiati, Daniele Barbaro, Salvatore Monti, Maurilio Deandrea, Laura Fugazzola, Giovanni Gambelunghe, Roberto Negro, Stefano Spiezia, Fulvio Stacul, Luca Maria Sconfien
Endocrine.2022; 76(1): 1. CrossRef - Image-Guided Percutaneous Ablation for Primary and Metastatic Tumors
Arian Mansur, Tushar Garg, Apurva Shrigiriwar, Vahid Etezadi, Christos Georgiades, Peiman Habibollahi, Timothy C. Huber, Juan C. Camacho, Sherif G. Nour, Alan Alper Sag, John David Prologo, Nariman Nezami
Diagnostics.2022; 12(6): 1300. CrossRef - Approach to FNA of Thyroid Gland Cysts
Esther Diana Rossi, Pietro Tralongo, Vincenzo Fiorentino, Mariangela Curatolo, Carmine Bruno, Carmen De Crea, Marco Raffaelli, Alfredo Pontecorvi, Luigi Maria Larocca
Advances in Anatomic Pathology.2022; 29(6): 358. CrossRef
- Ultrasound-guided ethanol ablation versus the Sistrunk operation as a primary treatment for thyroglossal duct cysts

- Clinical Study
- The Association of Overt and Subclinical Hyperthyroidism with the Risk of Cardiovascular Events and Cardiovascular Mortality: Meta-Analysis and Systematic Review of Cohort Studies
- Seo Young Sohn, Eunyoung Lee, Min Kyung Lee, Jae Hyuk Lee
- Endocrinol Metab. 2020;35(4):786-800. Published online November 25, 2020
- DOI: https://doi.org/10.3803/EnM.2020.728

- 6,189 View
- 289 Download
- 20 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Whether hyperthyroidism is an independent risk factor for cardiovascular events remains controversial. We aimed to evaluate the association of overt and subclinical hyperthyroidism with the risk of ischemic heart disease (IHD), stroke, heart failure, and cardiovascular mortality.
Methods
Studies regarding the association between hyperthyroidism and cardiovascular events were searched on PubMed and Embase databases. The cardiovascular disease (CVD) risk was classified as high and low, based on pre-existing diseases, including history of coronary, cerebral, or peripheral artery disease; heart failure; atrial fibrillation; diabetes mellitus; or chronic kidney disease.
Results
Thirty-seven cohort studies were included in this meta-analysis. The pooled hazard ratio for subjects with overt hyperthyroidism compared with the control group was 1.11 (95% confidence interval [CI], 1.03 to 1.19) for IHD, 1.35 (95% CI, 1.03 to 1.75) for stroke, and 1.20 (95% CI, 1.00 to 1.46) for cardiovascular mortality. For subjects with subclinical hyperthyroidism, the pooled hazard ratio was 1.24 (95% CI, 1.07 to 1.45) for IHD, when compared with the control group. Subgroup analysis by CVD risk showed that the risk of stroke in overt hyperthyroidism was increased in the low CVD risk group; however, these association was not observed in the high CVD risk group. Similarly, the risk of IHD in subjects with subclinical hyperthyroidism was significantly increased in the low CVD risk group.
Conclusion
Overt hyperthyroidism is associated with increased risk of IHD, stroke, and cardiovascular mortality, and subclinical hyperthyroidism is associated with increased risk of IHD. These associations were particularly observed in the low risk CVD group without underlying CVD. -
Citations
Citations to this article as recorded by- Trends in Prevalence of Thyroid Dysfunction and its Associations With Mortality Among US Participants, 1988-2012
Xiaowen Zhang, Yong Wang, Hongwei Wang, Xinlin Zhang
The Journal of Clinical Endocrinology & Metabolism.2024; 109(2): e657. CrossRef - Adequacy of thyroid hormone replacement for people with hypothyroidism in real‐world settings: A systematic review and meta‐analysis of observational studies
Agathoklis Efthymiadis, Matthew Henry, Dimitrios Spinos, Marianthi Bourlaki, Alexandros Tsikopoulos, Angeliki Bourazana, Anastasios Bastounis, Konstantinos Tsikopoulos
Clinical Endocrinology.2024; 100(5): 488. CrossRef - Thyroid Disorders and Peripheral Arterial Disease
Katica Bajuk Studen, Simona Gaberscek, Katja Zaletel, Ales Blinc, Miso Sabovic, Gerit-Holger Schernthaner, Panagiotis Anagnostis, Pier Luigi Antignani, Mojca Jensterle, Dimitri P Mikhailidis, Pavel Poredos
Current Vascular Pharmacology.2024; 22(1): 36. CrossRef - Hormonal influences on cerebral aneurysms: unraveling the complex connections
Zahra Hasanpour Segherlou, Mahdieh Shakeri-Darzekonani, Armin Khavandegar, Sara Stephenson, Kimberly Ciccone, Forough Masheghati, Mohammad Reza Hosseini Siyanaki, Mac Lyerly, Brandon Lucke-Wold
Expert Review of Endocrinology & Metabolism.2024; 19(3): 207. CrossRef - Pulmonary Embolism in Patients Admitted With Takotsubo Cardiomyopathy: Prevalence and Associated In-Hospital Adverse Events
Omar Elkattawy, Antonia Sames, Sruthi Kunamneni , Riya Sutariya , Mohamed Ismail, Omar Mohamed , Thomas J Lee, Jahanzeb Javed, Sherif Elkattawy, Afif Hossain, Fayez Shamoon
Cureus.2024;[Epub] CrossRef - Higher Risk of Incident Hyperthyroidism in Patients With Atrial Fibrillation
Pang-Shuo Huang, Jen-Fang Cheng, Jien-Jiun Chen, Yi-Chih Wang, Juey-Jen Hwang, Cho-Kai Wu, Chia-Ti Tsai
The Journal of Clinical Endocrinology & Metabolism.2023; 109(1): 92. CrossRef - Eurasian clinical guidelines for the diagnosis and treatment of secondary (symptomatic) forms of arterial hypertension (2022)
I. E. Chazova, N. M. Chikhladze, N. V. Blinova, Zh. E. Belaya, N. M. Danilov, E. M. Elfimova, A. Yu. Litvin, L. Ya. Rozhinskaya, N. Yu. Sviridenko, M. Yu. Shvetsov, V. A. Azizov, E. A. Grigorenko, N. P. Mit’kovskaja, I. I. Mustafaev, A. G. Polupanov, A. S
Eurasian heart journal.2023; (1): 6. CrossRef -
Sympathetic Activation Promotes Cardiomyocyte Apoptosis in a Rabbit Susceptibility Model of Hyperthyroidism-Induced Atrial Fibrillation via the p38 MAPK Signaling Pathway
Jialin Zheng, Shijian Zhao, Qishi Yang, Yantao Wei, Jianmei Li, Tao Guo
Critical Reviews in Eukaryotic Gene Expression.2023; 33(5): 17. CrossRef - Cardiovascular outcomes in subclinical thyroid disease: an update
Matthew D. Ettleson
Current Opinion in Endocrinology, Diabetes & Obesity.2023; 30(5): 218. CrossRef - Lower free triiodothyronine levels are associated with higher all-cause and cardiovascular mortality in people with diabetes-NHANES 2007–2012
Chang Liu, Zhong Xin, Lin Hua
Diabetes Research and Clinical Practice.2023; 202: 110811. CrossRef - Hyperthyroidism
Sun Y. Lee, Elizabeth N. Pearce
JAMA.2023; 330(15): 1472. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef - Risks of suboptimal and excessive thyroid hormone replacement across ages
U. Feldt-Rasmussen, G. Effraimidis, S. Bliddal, M. Klose
Journal of Endocrinological Investigation.2023; 47(5): 1083. CrossRef - Association of Mild Thyroid Dysfunction and Adverse Prognosis Among Chinese Patients With Acute ST Segment Elevation Myocardial Infarction
Mei-Fang Li, Ze-Tao Wei, Shuai Li, Qi-Ming Feng, Jing-Bo Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Cardiovascular Effects of Subclinical Hyperthyroidism following Percutaneous Coronary Intervention
Ricardo Correa, Ricardo Villela
Clinical Thyroidology.2022; 34(6): 240. CrossRef - Weight Gain and Body Composition Changes during the Transition of Thyroid Function in Patients with Graves’ Disease Undergoing Radioiodine Treatment
Zhenqin Cai, Qiyu Chen, Yan Ling, Henrik Falhammar
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Minor perturbations of thyroid homeostasis and major cardiovascular endpoints—Physiological mechanisms and clinical evidence
Patrick Müller, Melvin Khee-Shing Leow, Johannes W. Dietrich
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Role of thyroid hormones-induced oxidative stress on cardiovascular physiology
María Laura Barreiro Arcos
Biochimica et Biophysica Acta (BBA) - General Subjects.2022; 1866(12): 130239. CrossRef - Yearly Incidence of Stroke and Bleeding in Atrial Fibrillation with Concomitant Hyperthyroidism: A National Discharge Database Study
Juqian Zhang, Arnaud Bisson, Grégoire Fauchier, Alexandre Bodin, Julien Herbert, Pierre Henri Ducluzeau, Gregory Y. H. Lip, Laurent Fauchier
Journal of Clinical Medicine.2022; 11(5): 1342. CrossRef - Platelet abnormalities in autoimmune thyroid diseases: A systematic review and meta-analysis
Yu-tian Cao, Kai-yu Zhang, Jing Sun, Yan Lou, Tian-su Lv, Xinyi Yang, Wen-hui Zhang, Jiang-yi Yu, Qi-biao Wu, Xi-qiao Zhou
Frontiers in Immunology.2022;[Epub] CrossRef - Subclinical Hyperthyroidism: A Review of the Clinical Literature
Karen Tsai, Angela M. Leung
Endocrine Practice.2021; 27(3): 254. CrossRef - Thyroid and heart, a clinically relevant relationship
G. Corona, L. Croce, C. Sparano, L. Petrone, A. Sforza, M. Maggi, L. Chiovato, M. Rotondi
Journal of Endocrinological Investigation.2021; 44(12): 2535. CrossRef - Antithyroid Drug Treatment in Graves’ Disease
Jae Hoon Chung
Endocrinology and Metabolism.2021; 36(3): 491. CrossRef - Cardiovascular Outcomes in Thyroid Cancer Patients Treated With Thyroidectomy: A Meta-Analysis
Eun Kyung Lee, Hwa Young Ahn, Eu Jeong Ku, Won Sang Yoo, Young Ki Lee, Kee-Hyun Nam, Young Jun Chai, Shinje Moon, Yuh-Seog Jung
The Journal of Clinical Endocrinology & Metabolism.2021;[Epub] CrossRef
- Trends in Prevalence of Thyroid Dysfunction and its Associations With Mortality Among US Participants, 1988-2012

- Clinical Study
- Long-Term Results of Thermal Ablation of Benign Thyroid Nodules: A Systematic Review and Meta-Analysis
- Se Jin Cho, Jung Hwan Baek, Sae Rom Chung, Young Jun Choi, Jeong Hyun Lee
- Endocrinol Metab. 2020;35(2):339-350. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.339

- 11,045 View
- 311 Download
- 39 Web of Science
- 47 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Ultrasound-guided thermal ablations have become one of the main options for treating benign thyroid nodules. To determine efficacy of thermal ablation of benign thyroid nodules, we performed a meta-analysis of studies with long-term follow-up of more than 3 years.
Methods
Databases were searched for studies published up to August 25, 2019, reporting patients with benign thyroid nodules treated with thermal ablation and with follow-up data of more than 3 years. Data extraction and quality assessment were performed according to PRISMA guidelines. The analysis yielded serial volume reduction rates (VRRs) of ablated nodules for up to 3 years or more, and adverse effect of ablation during follow-up. Radiofrequency ablation (RFA) and laser ablation (LA) were compared in a subgroup analysis.
Results
The pooled VRRs for ablated nodules showed rapid volume reduction before 12 months, a plateau from 12 to 36 months, and more volume reduction appearing after 36 months, demonstrating long-term maintenance of treatment efficacy. Thermal ablation had an acceptable complication rate of 3.8%. Moreover, patients undergoing nodule ablation showed no unexpected delayed complications during the follow-up period. In the subgroup analysis, RFA was shown to be superior to LA in terms of the pooled VRR and the number of patients who underwent delayed surgery.
Conclusion
Thermal ablations are safe and effective methods for treating benign thyroid nodules, as shown by a long follow-up analysis of more than 3 years. In addition, RFA showed superior VRRs compared with LA for the treatment of benign thyroid nodules, with less regrowth and less delayed surgery. -
Citations
Citations to this article as recorded by- Five-year follow-up results of thermal ablation for benign thyroid nodules: Systematic review and meta-analysis
Xidong Xu, Ying Peng, Guoxin Han
American Journal of Otolaryngology.2024; 45(1): 104025. CrossRef - Radiofrequency Ablation for Benign Nodules and for Cancer, Too?
Jonathon O. Russell, Kaitlyn M. Frazier
Otolaryngologic Clinics of North America.2024; 57(1): 83. CrossRef - An anthropomorphic thyroid phantom for ultrasound‐guided radiofrequency ablation of nodules
Tim Boers, Wyger Brink, Leonardo Bianchi, Paola Saccomandi, Johan van Hespen, Germen Wennemars, Sicco Braak, Michel Versluis, Srirang Manohar
Medical Physics.2024; 51(2): 826. CrossRef - The safety and efficacy of radiofrequency ablation in benign pediatric thyroid disease in the US: An initial case series
Grace S. Kim, Hilary Seeley, Julia Noel, Iram Ahmad, Kara Meister
Laryngoscope Investigative Otolaryngology.2024;[Epub] CrossRef - Radioiodine versus radiofrequency ablation to treat autonomously functioning thyroid nodules: a systematic review and comparative meta-analysis
Luca Giovanella, Maria Luisa Garo, Alfredo Campenní, Petra Petranović Ovčariček
European Journal of Nuclear Medicine and Molecular Imaging.2024;[Epub] CrossRef - Novel and Advanced Ultrasound Techniques for Thyroid Thermal Ablation
Wai-Kin Chan, Jui-Hung Sun, Miaw-Jene Liou, Chia-Jung Hsu, Yu-Ling Lu, Wei-Yu Chou, Yan-Rong Li, Feng-Hsuan Liu
Endocrinology and Metabolism.2024; 39(1): 40. CrossRef - Sublethal thermal stress promotes migration and invasion of thyroid cancer cells
Chi-Yu Kuo, Chung-Hsin Tsai, Jun Kui Wu, Shih-Ping Cheng, Yi-Hsien Hsieh
PLOS ONE.2024; 19(2): e0298903. CrossRef - The Role of Radiofrequency Ablation in Benign and Malignant Thyroid Nodules
Meghal Shah, Catherine McManus
Surgical Clinics of North America.2024;[Epub] CrossRef - Comparison of ultrasound-guided microwave ablation, laser ablation, and radiofrequency ablation for the treatment of elderly patients with benign thyroid nodules: A meta-analysis
Ying Qian, Zheng Li, Chunyun Fan, Yong Huang
Experimental Gerontology.2024; 191: 112425. CrossRef - Assessing the relative effectiveness of various ultrasound-guided ablation techniques for treating benign thyroid nodules: A systematic review and network meta-analysis
Xiangmei Sun, Jiaojiao Chen, Yan Zou, Jiahao Lei, Weizong Liu
Medicine.2024; 103(18): e38014. CrossRef - Benign Thyroid Nodules Respond Better to Thermal Ablation Retreatment If They Are Smaller
Iram Hussain
Clinical Thyroidology®.2024; 36(5): 199. CrossRef - Ultrasound imaging in thyroid nodule diagnosis, therapy, and follow‐up: Current status and future trends
Tim Boers, Sicco J. Braak, Nicole E. T. Rikken, Michel Versluis, Srirang Manohar
Journal of Clinical Ultrasound.2023; 51(6): 1087. CrossRef - Ultrasound (US)-Guided Ablation of Thyroid Nodules
Byung Seup Kim
Journal of Surgical Ultrasound.2023; 10(1): 14. CrossRef - Ultrasound-Guided Radiofrequency Ablation versus Thyroidectomy for the Treatment of Benign Thyroid Nodules in Elderly Patients: A Propensity-Matched Cohort Study
L. Yan, X.Y. Li, Y. Li, Y. Luo
American Journal of Neuroradiology.2023; 44(6): 693. CrossRef - Minimally Invasive Ablative Treatments for Benign Thyroid Nodules: Current Evidence and Future Directions
Enrico Papini, Laszlo Hegedüs
Thyroid®.2023; 33(8): 890. CrossRef - Influence factors and nomogram for volume reduction rate in benign thyroid nodule after thermal ablation
Shiliang Cao, Lijia Wang, Ying Wei, Zhenlong Zhao, Jie Wu, Mingan Yu
International Journal of Hyperthermia.2023;[Epub] CrossRef - Choice in Ablative Therapies for Thyroid Nodules
Q Lina Hu, Jennifer H Kuo
Journal of the Endocrine Society.2023;[Epub] CrossRef - 2022 Taiwan clinical multicenter expert consensus and recommendations for thyroid radiofrequency ablation
Wei-Che Lin, Wen-Chieh Chen, Pei-Wen Wang, Yi-Chia Chan, Yen-Hsiang Chang, Harn-Shen Chen, Szu-Tah Chen, Wei-Chih Chen, Kai-Lun Cheng, Shun-Yu Chi, Pi-Ling Chiang, Chen-Kai Chou, Feng-Fu Chou, Shun-Chen Huang, Feng-Hsuan Liu, Sheng-Dean Luo, Fen-Yu Tseng,
Ultrasonography.2023; 42(3): 357. CrossRef - Comparison of the Efficiency of Radiofrequency and Microwave Ablation Methods in the Treatment of Benign Thyroid Nodules
Mahi N. Cerit, Cem Yücel, Ethem T. Cerit, Mehmet M. Yalçın, Halit N. Şendur, Suna Ö. Oktar
Academic Radiology.2023; 30(10): 2172. CrossRef - Radiofrequency ablation for autonomously functioning nodules as treatment for hyperthyroidism: subgroup analysis of toxic adenoma and multinodular goitre and predictors for treatment success
M. M. D. van der Meeren, F. B. M. Joosten, S. H. P. P. Roerink, L. N. Deden, W. J. G. Oyen
European Journal of Nuclear Medicine and Molecular Imaging.2023; 50(12): 3675. CrossRef - Massive Hemorrhage and Mortality Following Thyroid Radiofrequency Ablation
Seulki Song, Jin Pyeong Kim
Ear, Nose & Throat Journal.2023;[Epub] CrossRef - Clinical Approach for Thyroid Radiofrequency Ablation
Jung Suk Sim
Journal of the Korean Society of Radiology.2023; 84(5): 1017. CrossRef - General Principles for the Safe Performance, Training, and Adoption of Ablation Techniques for Benign Thyroid Nodules: An American Thyroid Association Statement
Catherine F. Sinclair, Jung Hwan Baek, Kathleen E. Hands, Steven P. Hodak, Timothy C. Huber, Iram Hussain, Brian Hung-Hin Lang, Julia E. Noel, Maria Papaleontiou, Kepal N. Patel, Gilles Russ, Jonathon Russell, Stefano Spiezia, Jennifer H. Kuo
Thyroid®.2023; 33(10): 1150. CrossRef - A comprehensive review of interventional ablation techniques for the management of thyroid nodules and metastatic lymph nodes
Jennifer H. Kuo, Catherine F. Sinclair, Brian Lang, Stefano Spiezia, Mingan Yu, Eun Ju Ha, Dong Gyu Na, Chiara Offi, Kepal N. Patel, Jung Hwan Baek
Surgery.2022; 171(4): 920. CrossRef - Radiofrequency ablation and related ultrasound‐guided ablation technologies for treatment of benign and malignant thyroid disease: An international multidisciplinary consensus statement of the American Head and Neck Society Endocrine Surgery Section with
Lisa A. Orloff, Julia E. Noel, Brendan C. Stack, Marika D. Russell, Peter Angelos, Jung Hwan Baek, Kevin T. Brumund, Feng‐Yu Chiang, Mary Beth Cunnane, Louise Davies, Andrea Frasoldati, Anne Y. Feng, Laszlo Hegedüs, Ayaka J. Iwata, Emad Kandil, Jennifer K
Head & Neck.2022; 44(3): 633. CrossRef - Assessment of thyroid-specific quality of life in patients with benign symptomatic thyroid nodules treated with radiofrequency or ethanol ablation: a prospective multicenter study
So Yeong Jeong, Eun Ju Ha, Jung Hwan Baek, Tae Yong Kim, Yu-Mi Lee, Jeong Hyun Lee, Jeonghun Lee
Ultrasonography.2022; 41(1): 204. CrossRef - Thyroid Nodule Radiofrequency Ablation: Complications and Clinical Follow Up
James Y. Lim, Jennifer H. Kuo
Techniques in Vascular and Interventional Radiology.2022; 25(2): 100824. CrossRef - Radiofrequency Ablation of Solid, Non-Functional Thyroid Nodules
Michael Douek
Techniques in Vascular and Interventional Radiology.2022; 25(2): 100821. CrossRef - Efficacy and Safety of Thermal Ablation for Treating Lymph Node Metastasis From Papillary Thyroid Carcinoma: A Systematic Review and Meta-Analysis
Zheng Ding, Juan Chen, Zhiguang Chen, Xiaoke Zeng, Pengchao Zheng, Xuemei Wang, Xinwu Cui, Liang Sang
Frontiers in Oncology.2022;[Epub] CrossRef - Intraoperative Neuromonitoring: Evaluating the Role of Continuous IONM and IONM Techniques for Emerging Surgical and Percutaneous Procedures
Catherine McManus, Jennifer Hong Kuo
Frontiers in Endocrinology.2022;[Epub] CrossRef - Thermal Ablation for the Management of Papillary Thyroid Microcarcinoma in the Era of Active Surveillance and Hemithyroidectomy
Sae Rom Chung, Jung Hwan Baek, Young Jun Choi, Jeong Hyun Lee
Current Oncology Reports.2022; 24(8): 1045. CrossRef - enhanced anarchic society optimization technique for the classification of ultrasound thyroid images using ILBP
D. Anitha, S. Sathya Priya
International journal of health sciences.2022; : 4713. CrossRef - Image-Guided Percutaneous Ablation for Primary and Metastatic Tumors
Arian Mansur, Tushar Garg, Apurva Shrigiriwar, Vahid Etezadi, Christos Georgiades, Peiman Habibollahi, Timothy C. Huber, Juan C. Camacho, Sherif G. Nour, Alan Alper Sag, John David Prologo, Nariman Nezami
Diagnostics.2022; 12(6): 1300. CrossRef - Efficacy and safety of ultrasound-guided microwave ablation versus surgical resection for Bethesda category IV thyroid nodules: A retrospective comparative study
Jingjing Yang, Ya Zhang, Xingjia Li, Yueting Zhao, Xue Han, Guofang Chen, Xiaoqiu Chu, Ruiping Li, Jianhua Wang, Fei Huang, Chao Liu, Shuhang Xu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Long-term follow-up of the radiofrequency ablation of benign thyroid nodules: the value of additional treatment
Hyun Jin Kim, Jung Hwan Baek, Woojin Cho, Jung Suk Sim
Ultrasonography.2022; 41(4): 661. CrossRef - Das „heiße“ Schilddrüsenkarzinom mit einem kritischen Blick auf die Thermoablation
Joachim Jähne, Andreas Niesen, Joachim Bernhardts, Marija Hillemans
Der Chirurg.2021; 92(1): 34. CrossRef - Current Practice of Percutaneous Ablation Technologies for Thyroid Nodules 2020
Haris Muhammad, Jonathon O. Russell, Prasanna Santhanam, Aniqa Tehreem, Ralph P. Tufano
Current Otorhinolaryngology Reports.2021; 9(1): 52. CrossRef - RFA and benign thyroid nodules: Review of the current literature
Haris Muhammad, Prasanna Santhanam, Jonathon O. Russell, Jennifer H. Kuo
Laryngoscope Investigative Otolaryngology.2021; 6(1): 155. CrossRef - Thermal Treatment Options for Benign Thyroid Nodules—The Role of Radio-Frequency Ablation and Laser Therapy
Erivelto Volpi
Clinical Thyroidology.2021; 33(1): 17. CrossRef - Comparative efficacy of different ultrasound-guided ablation for the treatment of benign thyroid nodules: Systematic review and network meta-analysis of randomized controlled trials
Linye He, Wanjun Zhao, Zijing Xia, Anping Su, Zhihui Li, Jingqiang Zhu, Ivan D. Florez
PLOS ONE.2021; 16(1): e0243864. CrossRef - Unresolved Clinical Issues in Thermal Ablation of Benign Thyroid Nodules: Regrowth at Long-Term Follow-Up
Jung Suk Sim, Jung Hwan Baek
Korean Journal of Radiology.2021; 22(8): 1436. CrossRef - Current Status and Challenges of US-Guided Radiofrequency Ablation of Thyroid Nodules in the Long Term: A Systematic Review
Stella Bernardi, Andrea Palermo, Rosario Francesco Grasso, Bruno Fabris, Fulvio Stacul, Roberto Cesareo
Cancers.2021; 13(11): 2746. CrossRef - Update of Radiofrequency Ablation for Treating Benign and Malignant Thyroid Nodules. The Future Is Now
Ralph P. Tufano, Pia Pace-Asciak, Jonathon O. Russell, Carlos Suárez, Gregory W. Randolph, Fernando López, Ashok R. Shaha, Antti Mäkitie, Juan P. Rodrigo, Luiz Paulo Kowalski, Mark Zafereo, Peter Angelos, Alfio Ferlito
Frontiers in Endocrinology.2021;[Epub] CrossRef - Factors Associated with the Efficacy of Radiofrequency Ablation in the Treatment of Benign Thyroid Nodules
Huynh Q Khanh, Nguyen L Vuong, Tran Q Tien
World Journal of Endocrine Surgery.2021; 12(3): 117. CrossRef - Long-Term Outcomes of Thermal Ablation for Benign Thyroid Nodules: The Issue of Regrowth
Jung Suk Sim, Jung Hwan Baek, Rosaria Meccariello
International Journal of Endocrinology.2021; 2021: 1. CrossRef - Matrix 3D ultrasound-assisted thyroid nodule volume estimation and radiofrequency ablation: a phantom study
T. Boers, S. J. Braak, M. Versluis, S. Manohar
European Radiology Experimental.2021;[Epub] CrossRef - Learning curve analysis of radiofrequency ablation for benign thyroid nodules
Chi-Yu Kuo, Chien-Liang Liu, Chung-Hsin Tsai, Shih-Ping Cheng
International Journal of Hyperthermia.2021; 38(1): 1536. CrossRef
- Five-year follow-up results of thermal ablation for benign thyroid nodules: Systematic review and meta-analysis

- Clinical Study
- Association between Circulating Irisin and C-Reactive Protein Levels: A Systematic Review and Meta-Analysis
- Elham Eslampour, Farzad Ebrahimzadeh, Amir Abbasnezhad, Mohammad Zeinali Khosroshahi, Razieh Choghakhori, Omid Asbaghi
- Endocrinol Metab. 2019;34(2):140-149. Published online June 24, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.2.140
- 4,610 View
- 53 Download
- 12 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Although previous studies have demonstrated that irisin plays an anti-inflammatory role in the body, conflicting results have been reported regarding the correlation between serum levels of irisin and C-reactive protein (CRP). The present meta-analysis was conducted to further investigate the correlation between irisin and CRP levels.
Methods We systematically searched PubMed, the Cochrane Library, Web of Science, Embase, SCOPUS, and Ovid to retrieve studies assessing the correlation between irisin and CRP levels. Meta-analyses were performed using a random-effects model, and the
I 2 index was used to evaluate heterogeneity.Results Of the 428 studies that were initially found, 14 studies with 2,530 participants met the inclusion criteria for the meta-analysis. The pooled effect size was calculated as 0.052 (95% confidence interval, −0.047 to 0.152;
P =0.302). Subgroup analyses identified s ignificant, positive, but weak correlations between CRP and irisin levels in cohort studies, studies conducted among healthy participants, studies in which the male-to-female ratio was less than 1, in overweight or obese subjects, and in studies with a sample size of at least 100 participants.Conclusion The present meta-analysis found no overall significant correlation between irisin and CRP levels, although a significant positive correlation was found in overweight or obese subjects. Well-designed studies are needed to verify the results of the present meta-analysis.
-
Citations
Citations to this article as recorded by- Zinc Supplementation in Individuals with Prediabetes and type 2 Diabetes: a GRADE-Assessed Systematic Review and Dose-Response Meta-analysis
Matin Nazari, Mahlagha Nikbaf-Shandiz, Fereshteh Pashayee-Khamene, Reza Bagheri, Kian Goudarzi, Navid Vahid Hosseinnia, Sina Dolatshahi, Hossein Salehi Omran, Niusha Amirani, Damoon Ashtary-larky, Omid Asbaghi, Matin Ghanavati
Biological Trace Element Research.2023;[Epub] CrossRef - Irisin reduces inflammatory signaling pathways in inflammation-mediated metabolic syndrome
John J. Slate-Romano, Naohiro Yano, Ting C. Zhao
Molecular and Cellular Endocrinology.2022; 552: 111676. CrossRef - Circulating Irisin Levels in Patients with Chronic Plaque Psoriasis
Francesca Ambrogio, Lorenzo Sanesi, Angela Oranger, Chiara Barlusconi, Manuela Dicarlo, Patrizia Pignataro, Roberta Zerlotin, Paolo Romita, Elvira Favoino, Gerardo Cazzato, Nicoletta Cassano, Gino Antonio Vena, Caterina Foti, Maria Grano
Biomolecules.2022; 12(8): 1096. CrossRef - Fibronectin type III domain-containing 5 in cardiovascular and metabolic diseases: a promising biomarker and therapeutic target
Xin Zhang, Can Hu, Hai-ming Wu, Zhen-guo Ma, Qi-zhu Tang
Acta Pharmacologica Sinica.2021; 42(9): 1390. CrossRef - Progress and Challenges in the Biology of FNDC5 and Irisin
Steffen Maak, Frode Norheim, Christian A Drevon, Harold P Erickson
Endocrine Reviews.2021; 42(4): 436. CrossRef - L-arginine supplementation to mitigate cardiovascular effects of walking outside in the context of traffic-related air pollution in participants with elevated blood pressure: A randomized, double-blind, placebo-controlled trial
Hongyu Li, Qisijing Liu, Zhiyong Zou, Qiao Chen, Wanzhou Wang, Andrea A. Baccarelli, Furong Deng, Xinbiao Guo, Shaowei Wu
Environment International.2021; 156: 106631. CrossRef - “Association between dietary inflammatory index (DII) and risk of irritable bowel syndrome: a case-control study”
Elham Eslampour, Koroush Ghanadi, Vahideh Aghamohammadi, Alireza Moayed Kazemi, Rasool Mohammadi, Farhad Vahid, Amir Abbasnezhad
Nutrition Journal.2021;[Epub] CrossRef - Roles and Mechanisms of Irisin in Attenuating Pathological Features of Osteoarthritis
Xiangfen Li, Xiaofang Zhu, Hongle Wu, Thomas E. Van Dyke, Xiaoyang Xu, Elise F. Morgan, Wenyu Fu, Chuanju Liu, Qisheng Tu, Dingming Huang, Jake Chen
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - Irisin, interleukin-33 and interleukin-37 in patients with ischemic heart disease and obesity
Yuliia Kovalova, Nataliia Sukhonos, Valeriia Brek, Kateryna Smolianyk
Medicinski casopis.2021; 55(3): 87. CrossRef - Effect of ursodeoxycholic acid therapy due to pregnant intrahepatic cholestasis on chemerin and irisin levels
Krzysztof Dąbrowski, Rafał Kierach, Beniamin O. Grabarek, Dariusz Boroń, Michał Kukla
Dermatologic Therapy.2020;[Epub] CrossRef - The effects of royal jelly and tocotrienol‐rich fraction on impaired glycemic control and inflammation through irisin in obese rats
Pardis Irandoost, Naimeh Mesri Alamdari, Atoosa Saidpour, Farzad Shidfar, Neda Roshanravan, Mohammad Asghari Jafarabadi, Farnaz Farsi, Nazanin Asghari Hanjani, Mohammadreza Vafa
Journal of Food Biochemistry.2020;[Epub] CrossRef - COVID-19: Could Irisin Become the Handyman Myokine of the 21st Century?
Alessia Catalano
Coronaviruses.2020; 1(1): 32. CrossRef - Effect of l-arginine supplementation on C-reactive protein and other inflammatory biomarkers: A systematic review and meta-analysis of randomized controlled trials
Behzad Nazarian, Ezatollah Fazeli Moghadam, Omid Asbaghi, Mohammad Zeinali Khosroshahi, Razieh Choghakhori, Amir Abbasnezhad
Complementary Therapies in Medicine.2019; 47: 102226. CrossRef - The effect of green tea on C-reactive protein and biomarkers of oxidative stress in patients with type 2 diabetes mellitus: A systematic review and meta-analysis
Omid Asbaghi, Faezeh Fouladvand, Michael J. Gonzalez, Vahideh Aghamohammadi, Razieh Choghakhori, Amir Abbasnezhad
Complementary Therapies in Medicine.2019; 46: 210. CrossRef
- Zinc Supplementation in Individuals with Prediabetes and type 2 Diabetes: a GRADE-Assessed Systematic Review and Dose-Response Meta-analysis

- Diabetes
- Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
- Jae Hyun Bae, Sunhee Kim, Eun-Gee Park, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
- Endocrinol Metab. 2019;34(1):80-92. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.80
- 7,737 View
- 267 Download
- 36 Web of Science
- 38 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background To investigate the effects of dipeptidyl peptidase-4 (DPP-4) inhibitors on renal outcomes in patients with type 2 diabetes.
Methods MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials were searched to identify randomized controlled trials (RCTs) of DPP-4 inhibitors from inception to September 2017. We selected eligible RCTs comparing DPP-4 inhibitors with placebo or other antidiabetic agents and reporting at least one renal outcome. A meta-analysis was conducted to calculate standardized mean differences, weighted mean differences (WMDs), relative risks (RRs), and 95% confidence intervals (CIs) for each renal outcome.
Results We included 23 RCTs with 19 publications involving 41,359 patients. Overall changes in urine albumin-to-creatinine ratio were comparable between DPP-4 inhibitors and controls (
P =0.150). However, DPP-4 inhibitors were associated with significantly lower risk of incident microalbuminuria (RR, 0.89; 95% CI, 0.80 to 0.98;P =0.022) and macroalbuminuria (RR, 0.77; 95% CI, 0.61 to 0.97;P =0.027), as well as higher rates of regression of albuminuria (RR, 1.22; 95% CI, 1.10 to 1.35;P <0.001) compared with controls. Although DPP-4 inhibitors were associated with small but significantly lower estimated glomerular filtration rate (WMD, −1.11 mL/min/1.73 m2; 95% CI, −1.78 to −0.44;P =0.001), there was no difference in the risk of end-stage renal disease between two groups (RR, 0.93; 95% CI, 0.76 to 1.14;P =0.475).Conclusion DPP-4 inhibitors had beneficial renal effects mainly by reducing the risk of development or progression of albuminuria compared with placebo or other antidiabetic agents.
-
Citations
Citations to this article as recorded by- Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study
Mototsugu Nagao, Jun Sasaki, Kyoko Tanimura-Inagaki, Ichiro Sakuma, Hitoshi Sugihara, Shinichi Oikawa
Cardiovascular Diabetology.2024;[Epub] CrossRef - Effects of glucose‐lowering agents on cardiovascular and renal outcomes in subjects with type 2 diabetes: An updated meta‐analysis of randomized controlled trials with external adjudication of events
Edoardo Mannucci, Marco Gallo, Andrea Giaccari, Riccardo Candido, Basilio Pintaudi, Giovanni Targher, Matteo Monami
Diabetes, Obesity and Metabolism.2023; 25(2): 444. CrossRef - Sitagliptin Mitigates Diabetic Nephropathy in a Rat Model of Streptozotocin-Induced Type 2 Diabetes: Possible Role of PTP1B/JAK-STAT Pathway
Sarah M. AL-Qabbaa, Samaher I. Qaboli, Tahani K. Alshammari, Maha A. Alamin, Haya M. Alrajeh, Lama A. Almuthnabi, Rana R. Alotaibi, Asma S. Alonazi, Anfal F. Bin Dayel, Nawal M. Alrasheed, Nouf M. Alrasheed
International Journal of Molecular Sciences.2023; 24(7): 6532. CrossRef - Take an individualized and multipronged approach when managing older adults with type 2 diabetes
Sheridan M. Hoy
Drugs & Therapy Perspectives.2023; 39(5): 171. CrossRef - Cardiovascular and Renal Outcomes With Sodium-Glucose Cotransporter-2 Inhibitors and Dipeptidyl Peptidase-4 Inhibitors Combination Therapy: A Meta-Analysis of Randomized Cardiovascular Outcome Trials
Awadhesh Kumar Singh, Akriti Singh, Ritu Singh
Endocrine Practice.2023; 29(7): 509. CrossRef - Sodium‐glucose cotransporter 2 inhibitors versus dipeptidyl peptidase 4 inhibitors on new‐onset overall cancer in Type 2 diabetes mellitus: A population‐based study
Cheuk To Chung, Ishan Lakhani, Oscar Hou In Chou, Teddy Tai Loy Lee, Edward Christopher Dee, Kenrick Ng, Wing Tak Wong, Tong Liu, Sharen Lee, Qingpeng Zhang, Bernard Man Yung Cheung, Gary Tse, Jiandong Zhou
Cancer Medicine.2023; 12(11): 12299. CrossRef - Comparative Effects of Glucose-Lowering Medications on Kidney Outcomes in Type 2 Diabetes
Deborah J. Wexler, Ian H. de Boer, Alokananda Ghosh, Naji Younes, Ionut Bebu, Silvio E. Inzucchi, Janet B. McGill, Sunder Mudaliar, David Schade, Michael W. Steffes, William V. Tamborlane, Meng H. Tan, Faramarz Ismail-Beigi, Jill P. Crandall, Melissa Dian
JAMA Internal Medicine.2023; 183(7): 705. CrossRef - SAFETY PROFILE OF DIPEPTIDYL PEPTIDASE-4 INHIBITORS
M. Ganeva
Trakia Journal of Sciences.2023; 21(1): 54. CrossRef - Chronic Kidney Disease and SGLT2 Inhibitors: A Review of the Evolving Treatment Landscape
Christian W. Mende
Advances in Therapy.2022; 39(1): 148. CrossRef - Management of Hyperglycemia in Older Adults with Type 2 Diabetes
Gunjan Y. Gandhi, Arshag D. Mooradian
Drugs & Aging.2022; 39(1): 39. CrossRef - Pharmacoeconomic evaluation of dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes mellitus: a systematic literature review
Zhen Ruan, Huimin Zou, Qing Lei, Carolina Oi Lam Ung, Honghao Shi, Hao Hu
Expert Review of Pharmacoeconomics & Outcomes Research.2022; 22(4): 555. CrossRef - Effect of Anagliptin versus Sitagliptin on Renal Function: Subanalyzes from the REASON Trial
Hiroki Teragawa, Takeshi Morimoto, Yuichi Fujii, Tomohiro Ueda, Mio Sakuma, Michio Shimabukuro, Osamu Arasaki, Koichi Node, Takashi Nomiyama, Shinichiro Ueda
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 685. CrossRef - Glomerular filtration rate as a kidney outcome of diabetic kidney disease: a focus on new antidiabetic drugs
Hyo Jin Kim, Sang Soo Kim, Sang Heon Song
The Korean Journal of Internal Medicine.2022; 37(3): 502. CrossRef - The Effects of Dipeptidyl Peptidase 4 Inhibitors on Renal Function in Patients with Type 2 Diabetes Mellitus
Wan-Chia Hsu, Chun-Sheng Lin, Jung-Fu Chen, Chih-Min Chang
Journal of Clinical Medicine.2022; 11(9): 2653. CrossRef - Treatment of diabetes mellitus has borne much fruit in the prevention of cardiovascular disease
Hiroaki Yagyu, Hitoshi Shimano
Journal of Diabetes Investigation.2022; 13(9): 1472. CrossRef - Finerenone, a Novel and Safer Approach toward Management of Diabetic Kidney Disease with Heart Failure
Ayesha Abdul Qadir Memon, Sarmad Iqbal
Global Journal of Medical, Pharmaceutical, and Biomedical Update.2022; 17: 12. CrossRef - The effects of dipeptidyl peptidase‐4 inhibitors on kidney outcomes
Daniel V. O'Hara, Thomas R. Parkhill, Sunil V. Badve, Min Jun, Meg J. Jardine, Vlado Perkovic
Diabetes, Obesity and Metabolism.2021; 23(3): 763. CrossRef - Urinary DPP4 correlates with renal dysfunction, and DPP4 inhibition protects against the reduction in megalin and podocin expression in experimental CKD
Acaris Benetti, Flavia Letícia Martins, Letícia Barros Sene, Maria Heloisa M. Shimizu, Antonio C. Seguro, Weverton M. Luchi, Adriana C. C. Girardi
American Journal of Physiology-Renal Physiology.2021; 320(3): F285. CrossRef - Incretin-based drugs and the kidney in type 2 diabetes: choosing between DPP-4 inhibitors and GLP-1 receptor agonists
Johannes F.E. Mann, Marcel H.A. Muskiet
Kidney International.2021; 99(2): 314. CrossRef - Renoprotective Effects of DPP-4 Inhibitors
Daiji Kawanami, Yuichi Takashi, Hiroyuki Takahashi, Ryoko Motonaga, Makito Tanabe
Antioxidants.2021; 10(2): 246. CrossRef - Danegaptide Prevents TGFβ1-Induced Damage in Human Proximal Tubule Epithelial Cells of the Kidney
Paul E. Squires, Gareth W. Price, Ulrik Mouritzen, Joe A. Potter, Bethany M. Williams, Claire E. Hills
International Journal of Molecular Sciences.2021; 22(6): 2809. CrossRef - Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2021; 36(2): 388. CrossRef - Consensus Recommendations by the Asian Pacific Society of Cardiology: Optimising Cardiovascular Outcomes in Patients with Type 2 Diabetes
Jack Wei Chieh Tan, David Sim, Junya Ako, Wael Almahmeed, Mark E Cooper, Jamshed J Dalal, Chaicharn Deerochanawong, David Wei Chun Huang, Sofian Johar, Upendra Kaul, Sin Gon Kim, Natalie Koh, Alice Pik-Shan Kong, Rungroj Krittayaphong, Bernard Kwok, Bien
European Cardiology Review.2021;[Epub] CrossRef - Diabetes and kidney disease: emphasis on treatment with SGLT-2 inhibitors and GLP-1 receptor agonists
Francesco Prattichizzo, Paola de Candia, Antonio Ceriello
Metabolism.2021; 120: 154799. CrossRef - SGLT2 Inhibitors and Other Novel Therapeutics in the Management of Diabetic Kidney Disease
Robert C. Stanton
Seminars in Nephrology.2021; 41(2): 85. CrossRef - Mineralocorticoid Receptor Antagonists in Diabetic Kidney Disease
Nina Vodošek Hojs, Sebastjan Bevc, Robert Ekart, Nejc Piko, Tadej Petreski, Radovan Hojs
Pharmaceuticals.2021; 14(6): 561. CrossRef - Podocyte Glucocorticoid Receptors Are Essential for Glomerular Endothelial Cell Homeostasis in Diabetes Mellitus
Swayam Prakash Srivastava, Han Zhou, Ocean Setia, Alan Dardik, Carlos Fernandez‐Hernando, Julie Goodwin
Journal of the American Heart Association.2021;[Epub] CrossRef - Coronavirus Disease (COVID)-19 and Diabetic Kidney Disease
Swayam Prakash Srivastava, Rohit Srivastava, Subhash Chand, Julie E. Goodwin
Pharmaceuticals.2021; 14(8): 751. CrossRef - Effects of DPP4 inhibitors on renal outcomes in diabetes mellitus: A systematic review and meta-analysis
SaikatK Dalui, Raja Chakraverty, Nafisha Yasmin, Smita Pattanaik, Kaushik Pandit, Suparna Chatterjee
Indian Journal of Endocrinology and Metabolism.2021; 25(4): 283. CrossRef - Comparison of Adverse Kidney Outcomes With Empagliflozin and Linagliptin Use in Patients With Type 2 Diabetic Patients in a Real-World Setting
Yueh-Ting Lee, Chien-Ning Hsu, Chung-Ming Fu, Shih-Wei Wang, Chiang-Chi Huang, Lung-Chih Li
Frontiers in Pharmacology.2021;[Epub] CrossRef - The Role of DPP-4 Inhibitors in Type-2 Diabetes Patients with Chronic Kidney Disease
Mishal Yousef Alqurashi, Khalid Faisal Alharthi, Abdulaziz Abdulrahman Alshehri, Yazeed Khalid Alharbi, Mohammad Abdulmunem Sanousi, Anas Abdullah Almazyed, Khulud Saeed Alghamdi, Sarah Musaad Alrashidi, Waad Abdullah Qaeed, Amjad Aedh Alasmari
Pharmacophore.2021; 12(3): 91. CrossRef - Type 2 diabetes mellitus management in patients with chronic kidney disease: an update
Zoi Kleinaki, Stella Kapnisi, Sofia-Andriani Theodorelou-Charitou, Ilias P. Nikas, Stavroula A. Paschou
Hormones.2020; 19(4): 467. CrossRef - Renal Outcomes in Type 2 Diabetes: A Review of Cardiovascular and Renal Outcome Trials
David M. Williams, Asif Nawaz, Marc Evans
Diabetes Therapy.2020; 11(2): 369. CrossRef - Favorable pleiotropic effects of sodium glucose cotransporter 2 inhibitors: head-to-head comparisons with dipeptidyl peptidase-4 inhibitors in type 2 diabetes patients
Shih-Chieh Shao, Kai-Cheng Chang, Swu-Jane Lin, Rong-Nan Chien, Ming-Jui Hung, Yuk-Ying Chan, Yea-Huei Kao Yang, Edward Chia-Cheng Lai
Cardiovascular Diabetology.2020;[Epub] CrossRef - Novel therapeutic agents for the treatment of diabetic kidney disease
Rachel E. Hartman, P.S.S. Rao, Mariann D. Churchwell, Susan J. Lewis
Expert Opinion on Investigational Drugs.2020; 29(11): 1277. CrossRef - Renal protection with glucagon-like peptide-1 receptor agonists
Martina Vitale, Jonida Haxhi, Tiziana Cirrito, Giuseppe Pugliese
Current Opinion in Pharmacology.2020; 54: 91. CrossRef - Loss of Mitochondrial Control Impacts Renal Health
Swayam Prakash Srivastava, Keizo Kanasaki, Julie E. Goodwin
Frontiers in Pharmacology.2020;[Epub] CrossRef - Effects of Sodium-Glucose Cotransporter 2 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Scientific Reports.2019;[Epub] CrossRef
- Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study

 KES
KES

 First
First Prev
Prev