Search
- Page Path
- HOME > Search
Review Article
- Diabetes, obesity and metabolism
- Glucagon-Like Peptide-1 Based Therapies: A New Horizon in Obesity Management
- Jang Won Son, Soo Lim
- Endocrinol Metab. 2024;39(2):206-221. Published online April 16, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1940
- 1,883 View
- 148 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
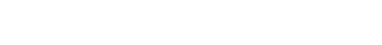
ePub - Obesity is a significant risk factor for health issues like type 2 diabetes and cardiovascular disease. It often proves resistant to traditional lifestyle interventions, prompting a need for more precise therapeutic strategies. This has led to a focus on signaling pathways and neuroendocrine mechanisms to develop targeted obesity treatments. Recent developments in obesity management have been revolutionized by introducing novel glucagon-like peptide-1 (GLP-1) based drugs, such as semaglutide and tirzepatide. These drugs are part of an emerging class of nutrient-stimulated hormone-based therapeutics, acting as incretin mimetics to target G-protein–coupled receptors like GLP-1, glucose-dependent insulinotropic polypeptide (GIP), and glucagon. These receptors are vital in regulating body fat and energy balance. The development of multiagonists, including GLP-1–glucagon and GIP–GLP-1–glucagon receptor agonists, especially with the potential for glucagon receptor activation, marks a significant advancement in the field. This review covers the development and clinical efficacy of various GLP-1-based therapeutics, exploring the challenges and future directions in obesity management.

Namgok Lecture 2022
- Diabetes, Obesity and Metabolism
- Incretin and Pancreatic β-Cell Function in Patients with Type 2 Diabetes
- Chang Ho Ahn, Tae Jung Oh, Se Hee Min, Young Min Cho
- Endocrinol Metab. 2023;38(1):1-9. Published online February 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.103

- 3,435 View
- 364 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - To maintain normal glucose homeostasis after a meal, it is essential to secrete an adequate amount of insulin from pancreatic β-cells. However, if pancreatic β-cells solely depended on the blood glucose level for insulin secretion, a surge in blood glucose levels would be inevitable after the ingestion of a large amount of carbohydrates. To avoid a deluge of glucose in the bloodstream after a large carbohydrate- rich meal, enteroendocrine cells detect the amount of nutrient absorption from the gut lumen and secrete incretin hormones at scale. Since insulin secretion in response to incretin hormones occurs only in a hyperglycemic milieu, pancreatic β-cells can secrete a “Goldilocks” amount of insulin (i.e., not too much and not too little) to keep the blood glucose level in the normal range. In this regard, pancreatic β-cell sensitivity to glucose and incretin hormones is crucial for maintaining normal glucose homeostasis. In this Namgok lecture 2022, we review the effects of current anti-diabetic medications on pancreatic β-cell sensitivity to glucose and incretin hormones.
-
Citations
Citations to this article as recorded by- Initial Combination Therapy in Type 2 Diabetes
Ji Yoon Kim, Nam Hoon Kim
Endocrinology and Metabolism.2024; 39(1): 23. CrossRef
- Initial Combination Therapy in Type 2 Diabetes

 KES
KES

 First
First Prev
Prev